Colorectal cancer is a type of cancer that affects the colon (large intestine) and the rectum. It is the third most common cancer in the world, after lung and breast cancer, and is responsible for approximately 9% of all cancer-related deaths. In this article, you will find causes, symptoms, diagnosis, treatment and prevention of colorectal cancer.
Statistics About Colorectal Cancer
Colorectal cancer is a significant global health issue, with millions of people affected by the disease each year. According to the World Health Organization (WHO), colorectal cancer is the third most common cancer worldwide with an estimated 1.8 million new cases and 861,000 deaths in 2018.
In the United States, colorectal cancer is the third most commonly diagnosed cancer in both men and women and it is the second leading cause of cancer-related deaths. In 2021, the American Cancer Society estimates that there will be 104,270 new cases of colon cancer and 45,230 new cases of rectal cancer in the United States.
The risk of developing colorectal cancer increases with age and the disease is most commonly diagnosed in people over the age of 50. But the incidence of colorectal cancer is increasing in younger adults, with a recent study showing that the incidence of colorectal cancer among adults aged 20 to 39 years has increased by 1% to 2.4% per year since the mid-1990s.


What is The Causes of Colorectal Cancer?
Certain cause of colorectal cancer is not fully understood but it is believed to be caused by a combination of genetic and environmental factors. Some of the factors that may increase the risk of developing colorectal cancer include:
- Age: Colorectal cancer is more common in people over the age of 50.
- Family History: People with a family history of colorectal cancer or polyps are at a higher risk of developing the disease.
- Inflammatory Bowel Disease: People with inflammatory bowel disease (IBD), such as Crohn’s disease or ulcerative colitis, have a higher risk of developing colorectal cancer.
- Lifestyle Factors: A diet that is high in fat and low in fiber, smoking, and heavy alcohol consumption may increase the risk of colorectal cancer.
- Obesity: People who are overweight or obese have an increased risk of developing colorectal cancer.
What Are The First Signs of Having Colon Cancer?
Here are some early signs of colorectal cancer:
- Changes in Bowel Habits: People with colorectal cancer may experience changes in their bowel habits, such as diarrhea, constipation or a change in the frequency or consistency of bowel movements. They may also feel like they need to have a bowel movement but are unable to do so. These changes can be lead to by a blockage in the colon or rectum, which can be a sign of cancer.
- Rectal Bleeding or Blood in the Stool: One of the most common signs of colorectal cancer is rectal bleeding or blood in the stool. The blood may be bright red or dark in color and may be mixed with the stool or appear on the toilet paper after wiping. In some cases, people with colorectal cancer may experience bleeding that is not visible to the naked eye, which can be detected through a stool test.
- Abdominal Pain or Cramping: People with colorectal cancer may experience abdominal pain or cramping, which can be a persistent discomfort or a sharp, crampy pain that comes and goes. This can be caused by a tumor that is growing in the colon or rectum and putting pressure on surrounding tissues.
- Weakness Or Fatigue: People with colorectal cancer may experience weakness or fatigue, which can be a general feeling of tiredness or weakness that does not improve with rest. This can be caused by the cancer itself, as well as by the body’s immune response to the cancer.
- Unexplained Weight Loss: People with colorectal cancer may experience unexplained weight loss, which can occur even without changes in diet or activity level. This can be caused by the cancer itself, as well as by a lack of appetite or nausea caused by the cancer.
- Anemia: People with colorectal cancer may experience anemia, which is a condition in which there is a shortage of red blood cells in the body. This can be a result of chronic bleeding from the cancer and can lead to symptoms such as weakness, fatigue and shortness of breath.
These symptoms can also be caused by other conditions, such as inflammatory bowel disease, hemorrhoids, or infections. However, if any of these symptoms persist or worsen, it’s important to consult a doctor to determine the underlying cause and receive appropriate treatment.
Diagnosis of Colorectal Cancer
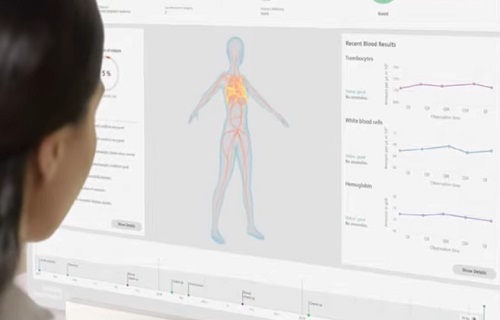
Diagnosis of colorectal cancer typically involves several steps, including a physical exam, medical history and diagnostic tests. These tests may include:
- Colonoscopy: Colonoscopy is a procedure that allows a doctor to examine the inside of the colon and rectum for signs of cancer or polyps.
- Biopsy: During a colonoscopy, a doctor may take a small tissue sample (biopsy) for examination under a microscope.
- Blood Tests: Blood tests may be used to check for signs of anemia or to look for tumor markers.
- Imaging Tests: Imaging tests, such as a CT scan, MRI or PET scan, may be used to look for signs of cancer in the colon and other parts of the body.
What Are The Treatment Ways of Colorectal Cancer?
Here are mostly used treatment ways for colorectal cancer:
- Surgery: Surgery is the most common treatment for colorectal cancer. The type of surgery depends on the location and stage of the cancer. In early-stage cancers, surgery may involve removing a small section of the colon or rectum. In more advanced cancers, surgery may involve removing a larger portion of the colon or rectum or even the entire colon or rectum. The surgeon may also remove nearby lymph nodes to check for the presence of cancer cells. After surgery, some patients may require a colostomy, which is a surgical opening in the abdominal wall that allows waste to pass through a bag attached to the skin.
- Radiation Therapy: Radiation therapy uses high-energy X-rays or other types of radiation to kill cancer cells. It may be used before surgery to shrink the tumor and make it easier to remove or after surgery to kill any remaining cancer cells. Radiation therapy can also be used to relieve symptoms in patients with advanced colorectal cancer.
- Chemotherapy: Chemotherapy uses drugs to kill cancer cells. It may be given before or after surgery or in combination with radiation therapy. Chemotherapy drugs can be given orally or intravenously and can be given in cycles, with a period of rest in between cycles. The side effects of chemotherapy can include nausea, vomiting, fatigue, hair loss and an increased risk of infection.
- Targeted Therapy: Targeted therapy uses drugs that target specific proteins or genes that are involved in the growth and spread of cancer cells. This type of therapy is often used in combination with chemotherapy or as a standalone treatment. Targeted therapy can have fewer side effects than chemotherapy but it can be expensive and may not be covered by insurance.
- Immunotherapy: Immunotherapy uses drugs that stimulate the body’s immune system to attack cancer cells. It is currently being studied as a treatment for colorectal cancer but is not yet widely used. Immunotherapy can have fewer side effects than chemotherapy or radiation therapy but it can be expensive and may not be covered by insurance.
- Palliative Care: Palliative care is an approach to care that focuses on relieving symptoms and improving quality of life for patients with advanced colorectal cancer. This may include pain management, nutritional support and counseling to address emotional and spiritual needs. Palliative care can be provided alongside other treatments for colorectal cancer, and can help patients and their families cope with the physical and emotional challenges of cancer treatment.
.
What Are Prevention Ways of Colorectal Cancer?
Here are some effective prevention strategies for colorectal cancer:
- Regular Screenings: Regular screenings are a key component of colorectal cancer prevention because they can detect polyps and other abnormalities in the colon and rectum before they become cancerous. There are several types of screening tests available, including colonoscopies, stool tests and virtual colonoscopies. Your doctor can help determine which screening method is best for you based on your age, family history and other risk factors.
- Healthy Diet: Healthy diet that is high in fruits, vegetables and whole grains and low in red and processed meats has been shown to reduce the risk of colorectal cancer. In particular, fiber-rich foods can help promote regular bowel movements and prevent constipation, which can reduce the risk of colorectal cancer. Some studies have also suggested that a diet rich in calcium and vitamin D may help lower the risk of colorectal cancer.
- Physical Activity: Regular physical activity can help maintain a healthy weight, which is an important factor in colorectal cancer prevention. Besides that physical activity has been shown to have a direct effect on colorectal cancer risk. Exercise can help improve digestion and bowel function, reduce inflammation and boost the immune system, all of which can lower the risk of colorectal cancer.
- Limit Alcohol Consumption: Drinking alcohol, especially in large amounts, has been linked to an increased risk of colorectal cancer. The risk appears to be highest among heavy drinkers but even moderate alcohol consumption can increase the risk. If you choose to drink alcohol, it’s recommended to do so in moderation.
- Don’t Smoke: Smoking cigarettes or using other tobacco products is a major risk factor for colorectal cancer, as well as many other types of cancer and other health problems. If you smoke, quitting is the best thing you can do for your health.
- Manage Chronic Conditions: Certain chronic conditions, such as inflammatory bowel disease (IBD) and type 2 diabetes, can increase the risk of colorectal cancer. If you have one of these conditions, it’s important to work with your doctor to manage it effectively and reduce your risk of developing colorectal cancer.
- Know Family History: If you have a family history of colorectal cancer, you may be at higher risk of developing the disease. In particular, if you have a first-degree relative (parent, sibling or child) who has had colorectal cancer or certain other cancers, you may be at increased risk. In some cases, genetic testing may be recommended to determine if you have an inherited risk for colorectal cancer. Your doctor can help you understand your family history and determine if additional screening or other preventive measures are needed.
What Are the Stage of Colorectal Cancer?
Here is some information about the different stages of colorectal cancer:
- Stage 0: This stage is often called “carcinoma in situ” because the cancer cells are still in the innermost layer of the colon or rectum lining, where they originated. This is the earliest stage of colorectal cancer and the cancer is usually small and localized. It’s often detected during a routine colonoscopy or other screening test and it has a very high cure rate.
- Stage I: In this stage, the cancer has grown beyond the innermost lining of the colon or rectum and has invaded the next layer of tissue. It has not yet spread to nearby lymph nodes or other organs. The cancer may be larger than in Stage 0, but it’s still usually small and localized. Surgery is usually the primary treatment for Stage I colorectal cancer and the cure rate is also very high.
- Stage II: In this stage, the cancer has grown through the outer layers of the colon or rectum and into nearby tissues. It has not yet spread to nearby lymph nodes or other organs. Cancer may be larger than in Stage I and it may be growing more aggressively. Surgery is also the primary treatment for Stage II colorectal cancer but the cancer may be more difficult to cure completely.
- Stage III: In this stage, the cancer has spread to nearby lymph nodes but has not yet spread to other organs. This is a more advanced stage of colorectal cancer and the cure rate is lower than in earlier stages. Treatment usually involves surgery, followed by chemotherapy to kill any remaining cancer cells.
- Stage IV: In this stage, the cancer has spread to distant organs, such as the liver, lungs or brain. This is the most advanced stage of colorectal cancer and the cure rate is very low. Treatment may involve surgery to remove as much of the cancer as possible, followed by chemotherapy and/or radiation therapy to slow the cancer’s growth and relieve symptoms.
Besides to the main stages of colorectal cancer, doctors may also use a sub-staging system to further classify the cancer and guide treatment decisions. The sub-staging system is based on the number of lymph nodes that are affected by the cancer, as well as other factors such as tumor size and location. The sub-stages are denoted by a letter (A, B, C, or D) and a number (1-4). For example, Stage III colon cancer may be further classified as Stage IIIB or IIIC, depending on the extent of lymph node involvement.



What is the survival rate of colorectal cancer?
According to the American Cancer Society, the overall 5-year relative survival rate for people with colorectal cancer is about 65%. This means that on average, people with colorectal cancer are 65% as likely as people without the disease to survive for at least 5 years after diagnosis.
But survival rates can vary widely change on the stage of the cancer at the time of diagnosis. For example, 5-year relative survival rate for people with localized colorectal cancer (meaning the cancer has not spread beyond the colon or rectum) is about 90%. But if the cancer has spread to distant parts of the body, the 5-year relative survival rate drops to about 14%.
What Is Colonoscopy Age Recommendations?
Age recommendations for colonoscopy screening vary slightly depending on the organization providing the guidelines but most recommend starting at age 45 or 50 for people at average risk of colorectal cancer. Here are some examples of age recommendations:
- American Cancer Society (ACS): The ACS recommends that people at average risk of colorectal cancer start regular screening at age 45. They recommend a range of screening tests, including colonoscopy, every 10 years.
- United States Preventive Services Task Force (USPSTF): The USPSTF recommends that people at average risk of colorectal cancer start regular screening at age 50 and continue until age 75. They recommend a range of screening tests, including colonoscopy, every 10 years.
- American College of Gastroenterology (ACG): The ACG recommends that people at average risk of colorectal cancer start regular screening at age 50 and continue until age 75. They recommend colonoscopy every 10 years as the preferred screening test.
We wish healthy days for you.